It is essential to understand hypoventilation and hyperventilation because they are two widespread breathing abnormalities for us with pectus excavatum.
We must learn to cope with them and understand why they arise because breathing issues and chest abnormalities like pectus excavatum are closely associated. Additionally, breathing problems can transform into panic and fear if we are unaware of why they occur.
Panic and fear can then become anxiety, also leading to breathing issues. This cycle can continue indefinitely. That is why it is crucial to be aware of any potential problem that could be connected to our deformity in some way.
What’s Hypoventilation?
A breathing problem known as respiratory depression (hypoventilation) is characterized by slow, inefficient breathing.
The body can’t efficiently expel carbon dioxide when hypoventilating. That may result in the lungs misusing oxygen. As a result, the body has too little oxygen and more carbon dioxide.
Hypoventilation can occur for many reasons, and chest wall deformities are one of them.
It results from decreased chest wall compliance caused by abnormal spine curvature, which is also often in chest malformations.
Symptoms
Depending on the problem’s severity, hypoventilation has various symptoms. Early signs may include mild, generalized symptoms like:
- Exhaustion
- Daytime tiredness and low energy
- Rapid breathing and breathing difficulties
But some signs could indicate a more severe form, such as:
- Confusion
- Disorientation
- Headaches and disruption in vision
- Increased sleepiness
- Having trouble remaining awake and sleeping for a long time at night
- Apnea or abnormally large breath gaps
- Strange breath sounds
What’s Hyperventilation and Its Symptoms?
Hyperventilation is the opposite of hypoventilation. That is when you breathe in more quickly than usual. This fast, deep breathing alters your lungs’ ability to exchange gases. You inhale oxygen and exhale carbon dioxide.
However, when you hyperventilate, you exhale more carbon dioxide than usual, which lowers blood levels of the gas. People aged 15 to 55 are most prone to hyperventilation. Women are more prone to this condition.
Hyperventilation and Pectus Study
A study on a 19-year-old boy with pectus excavatum shows the presence of hyperventilation.
Symptoms are comparable to hypoventilation and shortness of breath due to the pectus deformity. Such symptoms are:
- Chest pain
- Instability
- Breathing difficulty
- Bloating and dry mouth
- Disruptions in sleep
- Numbness in your mouth or your arms
- Hands and foot muscle spasms
Hypoventilation vs. Hyperventilation
Both issues can be disturbing. They can worry us to the point where we think our condition is worsening. However, these sensations can also happen in a completely healthy person. It is essential to act and recognize them in time. Be patient, and please don’t panic immediately if you feel some symptoms.
A person may occasionally appear to be hyperventilating when they are taking many shallow breaths. In many cases, learning how to breathe correctly can fix both problems.
These breathing problems are not a disease, but if the symptoms are frequent, it may be some form of a disorder that needs medical treatment.
People’s Experiences
Reddit is a place where a lot of pectus excavatum-related problems that are more or less known are shared. There are also comments from people who have experienced some form of hyperventilation or hypoventilation.
Most often, these problems are experienced during sports, especially running. Increased ventilation and fatigue appear soon after starting the activity.
Some of the people shared their worst experiences of hyperventilating.
They say it gets worse to the point where they feel their lungs are being destroyed. However, this can also be due to a lack of general fitness. That is why working out and gradually improving your physical shape is essential if you have pectus excavatum.
Home treatment
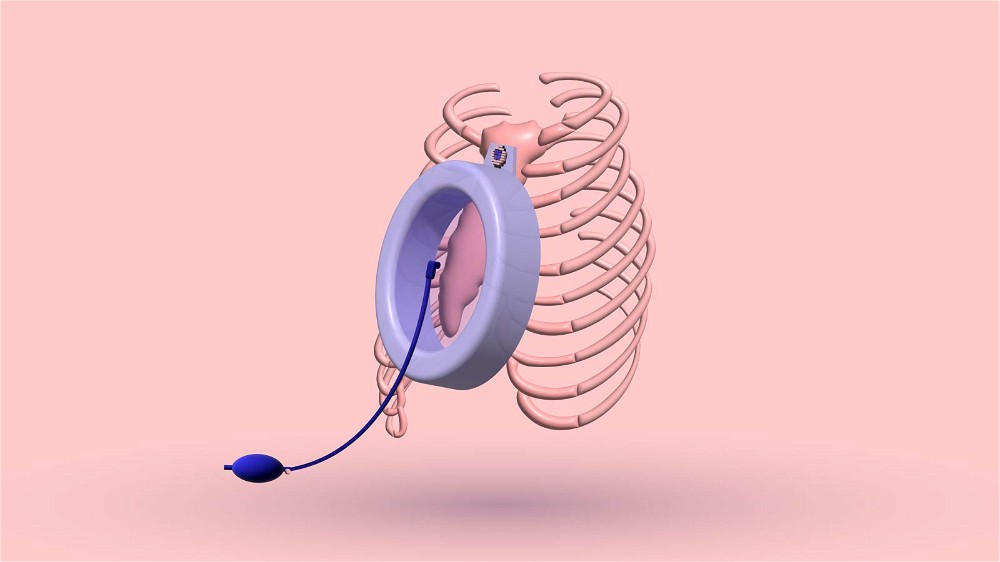
All home treatments imply proper breathing, a general topic concerning pectus excavatum deformities.
- Breathe with your lips pursed as if whistling.
Slow your breathing to one breath every five seconds, or slow enough that symptoms fade gradually.
- Belly breathing
Belly (diaphragmic) breathing fills your lungs, reduces your breathing rate, and allows you to rest.
Place one hand on your stomach, below the ribcage, and your other hand on your chest.
You can perform this while standing, although lying on the floor with your knees bent may be more comfortable.
Breathe deeply through your nose. Allow the belly to push your hand out as you breathe in, and try to maintain your chest’s stillness.
Repeat these steps 3–10 times. Take your time with each inhalation and see how the symptoms go away.
- Practice relaxation methods that suit you best, such as muscle relaxation, yoga movements, or meditation.
- Exercise daily and improve your physical condition
Be careful and choose your treatment wisely.
There are also many home treatments with a paper bag for hyperventilation on the internet.
It is claimed to be beneficial, but please, if you have other heart or lung problems due to your sunken chest, do not try these techniques before talking to a doctor. It is best to stick to the essential few types of breathing.
When to call a doctor?
Call a doctor if you experience a lot of chest pain, including squeezing (like a weight on the chest) or sharp and stabbing pain, especially if it worsens with deep breaths and if you are in fear and panic in such moments.
It is best to have someone by your side or call a loved one who will manage to calm you down at first. But immediately after that, please seek medical help so the condition does not worsen.
The Bottom Line
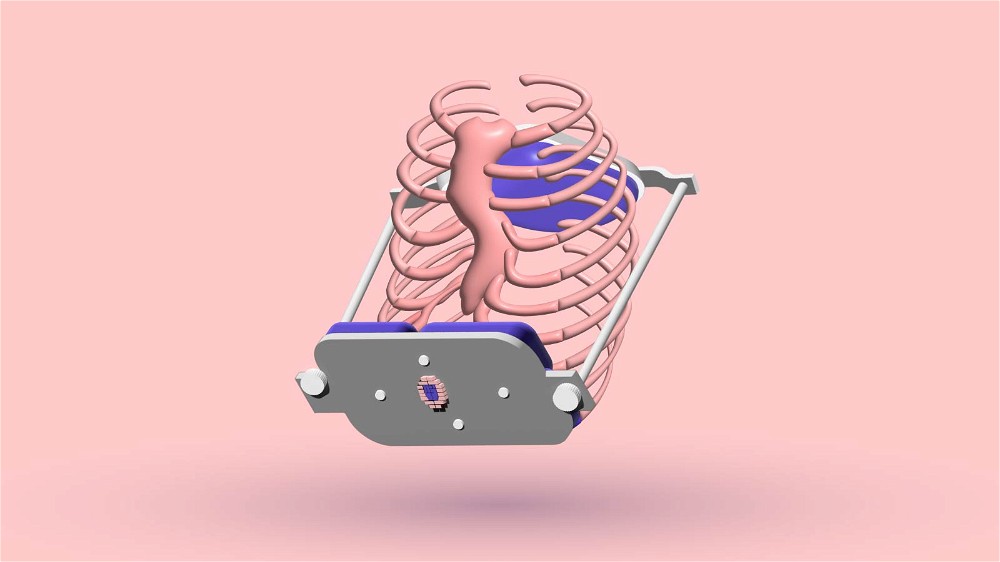
Living with pectus excavatum can involve a lot of troubled and irregular breathing.
Breathing is an automatic process; we don’t have to think about it. However, certain circumstances or chest malformations might alter our breathing rhythm, leaving us feeling out of breath, agitated, or on the point of passing out in the worst cases.
Hyperventilation and hypoventilation can be some of the most common breathing problems if you have pectus excavatum. It is ideal for identifying these problems and reporting them to your doctor. Both issues can cause problems in the long run, and you shouldn’t leave them untreated.
You will feel much more relieved knowing you don’t have those problems. I hope this blog post was beneficial to you and helped you. Thank you for reading!
10 Sources
- Hyperventilation | Johns Hopkins Medicine [Internet]. [cited 2022 Dec 8]. Available from: https://www.hopkinsmedicine.org/health/conditions-and-diseases/hyperventilation
- Respiratory Depression: Symptoms, Causes, and Treatments [Internet]. [cited 2022 Dec 8]. Available from: https://www.healthline.com/health/respiratory-depression
- Wada H, Kimura M, Shirahama R, Ikeda A, Gozal D, Tanigawa T. Pectus excavatum is associated with sleep-related breathing disorders in children. Eur Respir J. 2019 Oct;54(4):1900524.
- Thorax Deformity - an overview | ScienceDirect Topics [Internet]. [cited 2022 Dec 8]. Available from: https://www.sciencedirect.com/topics/pharmacology-toxicology-and-pharmaceutical-science/thorax-deformity
- Respiratory Depression (Hypoventilation): Definition, Symptoms, Traits, Causes, Treatment [Internet]. [cited 2022 Dec 8]. Available from: https://www.verywellmind.com/respiratory-depression-hypoventilation-definition-symptoms-traits-causes-treatment-5116903
- Hyperventilation: Symptoms, Causes, Treatment, Emergencies [Internet]. [cited 2022 Dec 8]. Available from: https://www.webmd.com/lung/lung-hyperventilation-what-to-do
- Wallaert B, Cavestri B, Fournier C, Nevière R, Aguilaniu B. Positional hyperventilation-induced hypoxaemia in pectus excavatum. Eur Respir J. 2006 Jul;28(1):243–7.
- Hyperventilation | HealthLink BC [Internet]. [cited 2022 Dec 8]. Available from: https://www.healthlinkbc.ca/health-topics/hyperventilation
- [cited 2022 Dec 8]. Available from: https://www.reddit.com/r/PectusExcavatum/comments/r8dxxt/do_you_guys_start_hyperventilating_faster_during/
- Hyperventilation: Care Instructions [Internet]. [cited 2022 Dec 8]. Available from: https://myhealth.alberta.ca:443/Health/aftercareinformation/pages/conditions.aspx?hwid=ut2508