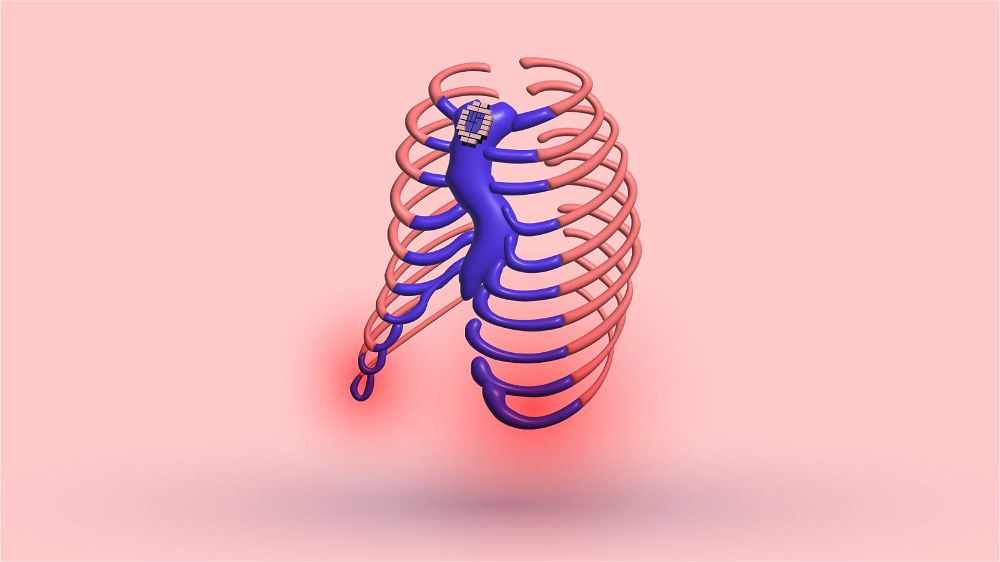
There are plenty of advantages of vacuum bell therapy over pectus excavatum surgery.
These advantages are enough for patients to choose this non-surgical treatment over minimally invasive procedures, especially if the deformity is mild or moderate.
List of Advantages
- Therapy is non-surgical
- Less restrictive
- Fewer side effects
- Freedom of the patient to determine the intensity of the application himself
- No ban on physical contact sports, such as in the case of the Nuss procedure
- No scars
- No blood loss
- Less pain
- Shorter treatment
- Airport beeping
1. Therapy is Non-Surgical
- There is no need for surgery preparation. That usually takes months or even years.
- No need for harmful X-Rays.
- Sometimes, the surgeon you want to do the surgery with has a full schedule, and you’ll need to wait a year or so. During this time, your deformity may worsen.
There is a lot of discomfort following a pectus excavatum surgery. This depends on which type of surgery was done. Post Ravitch or Nuss surgery, patients usually experience:
- The surgery is excruciating and will limit your physical activity for around three months.
- Nausea and vomiting as a result of the general anesthesia
- Soreness, pain, and swelling in the chest area
- Restlessness and sleeplessness
- Chest pain that doesn’t go away after a month or more
- Surgery-induced opioid addiction
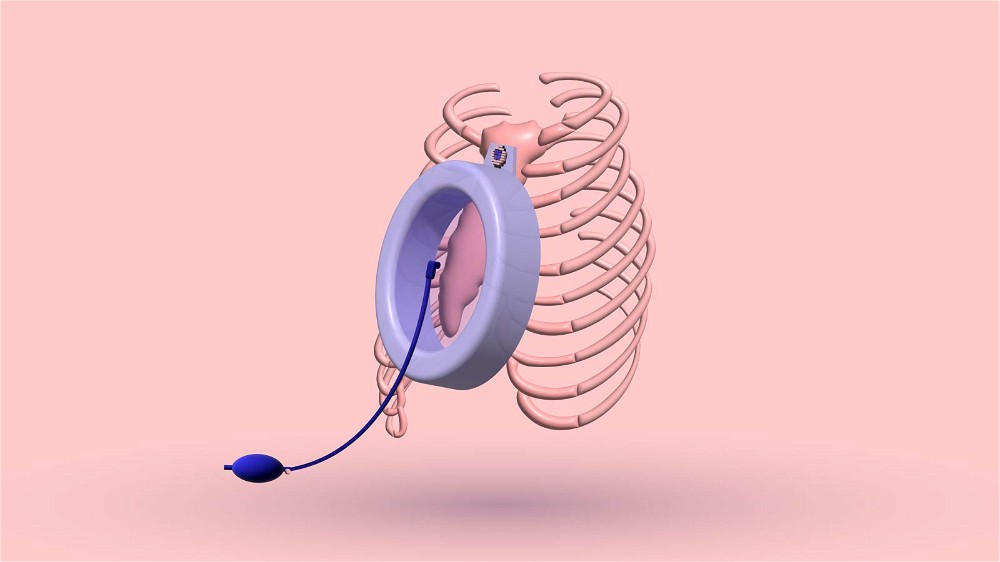
2. Less Restrictive
The suction bell can be removed at any time of the day, and you can continue playing your favorite sport with your buddies.
After that, you can put on the vacuum bell again. There is a lot of room for creativity.
That isn’t the case with the surgery. Removing the pectus bars will require additional surgery.
3. Fewer Side Effects

The potential side effects of vacuum bell therapy are:
- Skin bruising and swelling
- Subcutaneous hematoma—ruptured blood capillaries
- Pain in the upper back
- Skin irritation
- A numb sensation in the arms
Most of the side effects affect the skin. You can prevent these side effects with a proper chest skin routine while applying the vacuum bell.
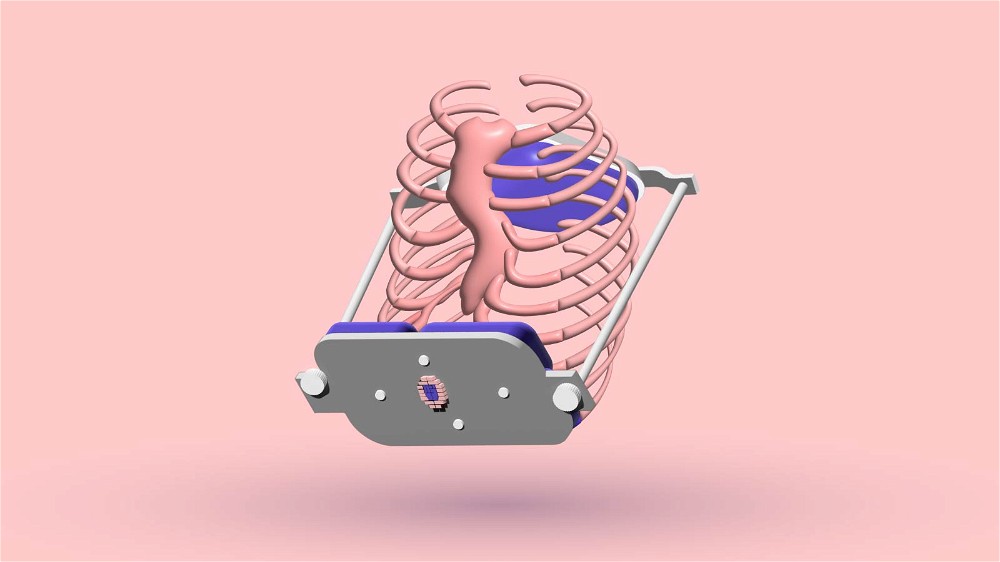
On the other hand, the side effects of Nuss surgery are:
- Infection
- Bleeding
- Pneumothorax
- Pleural effusion
- Inflammation around the heart - Pericarditis
- Bar displacement
- Cardiac injuries
- Risk of death
4. Less Pain
The pain is minimal in comparison to surgery. For example, if the pain becomes very uncomfortable, you can take off the suction bell for a moment. I don’t feel pain unless I pump the vacuum bell too hard.
You don’t need to pump until your sternum touches the transparent window. This is excessive and can even cause skin rashes and blisters. It can take a few months until the pain of the Nuss and Ravitch procedure disappears.
The pain of the vacuum bell, even when pushed to the limits, isn’t too bad for a painkiller.
5. Freedom to Determine the Intensity
On some days, you may feel more motivated to correct your pectus excavatum deformity with the vacuum bell. On those days, you can push the limits of the vacuum bell to the point where your sunken chest is close to the transparent window.
You can play it cool and pump just a few times on other days so your chest stays flattened. I did this while I went to sleep with the vacuum bell applied to sleep comfortably while I corrected the chest.
6. No Scars
At the end of the vacuum bell treatment, there are no scars. This isn’t the case with Nuss and Ravitch procedures.
Some patients that underwent the Ravitch procedure are more dissatisfied with the new scar in the center of their chest than the way their sunken chest looked previously.
7. No Blood Loss
Massive bleeding from a Nuss procedure is rare, but it may require a blood transfusion if it happens.
However, if this occurs, it can be fatal. Blood loss is expected in more invasive surgeries like the Ravitch procedure. This risk doesn’t exist with vacuum bell therapy.
8. No Physical Contact Sports Limit
There are a lot of physical restrictions following a Nuss procedure, which will lower your quality of life for a few months.
You should avoid full-contact sports such as football, rugby, ice hockey, and some martial arts for three years or until your Nuss bar is removed from your chest. These sports can cause bar dislocation in your chest, which can rupture your organs, such as the heart, or cut a major blood vessel.
This can be very demotivating for younger athletes who love to pursue a career in those sports. The Nuss procedure can break their dreams.
Concerning the vacuum bell, you can take it off any time you participate in these sports. You don’t have any bars in the chest, which can cause problems if you get struck.
9. Shorter Treatment
Usually, the vacuum bell needs to be used for about a year or until you’re satisfied with the results. If you use the device consistently, you will not need more than a year to finish the treatment successfully.
On the other hand, the Nuss bars usually stay in your chest for three years and require additional surgery to remove the bars.
10. Airport Beeping
The Nuss bar in your chest can cause the metal detector at the airport to beep. You will need to always carry a clinical letter at airports.
This can be unpleasant and complicate your travel if you can’t find the letter. This isn’t the case with the vacuum bell.
Vacuum Bell Is Not Perfect
It takes time and discipline if you want lasting success with the vacuum bell. You need to apply the device consistently. As an adult or teenager, you must clench your jaw and go on.
You must continue the treatment for at least six months.
Unfortunately, some patients think there is no correction and become impatient. Usually, there are no doctors to motivate them to continue the therapy.
Because of that, it is essential to be a part of a pectus excavatum group to interact with others.
Motivation Boost
Most recently, doctors can use an Optical Scanning Device for impatient patients to notice the differences before and after the vacuum bell treatment.
The goal of this approach is to keep these patients motivated.
The Bottom Line
The vacuum bell has a lot of advantages over pectus excavatum surgeries. The risks are minimal, while there are a lot of benefits.
Unfortunately, surgery may be the only option to correct a sunken chest in some severe cases fully. The vacuum bell is a perfect alternative to surgery if the deformity is mild or moderate.
If you have any questions or problems regarding the suction bell therapy and have nobody to get in touch with, please feel free to contact me personally.
I will respond and try to help you with your situation.
9 Sources
- X-rays: Overview, side effects, risks, and more [Internet]. [cited 2022 Nov 27].
Available from: https://www.medicalnewstoday.com/articles/219970#side-effects - Vacuum Bell Therapy: Does It Cure Pectus Excavatum? [Internet]. Cosmetic Surgery Nottingham & Plastic Surgery from Stephen McCulley. [cited 2022 Nov 27].
Available from: https://www.stephenmcculley.co.uk/resource-centre/other-procedures/vacuum-bell-therapy-cure-pectus-excavatum/ - Risks of Nuss procedure (pectus surgery) [Internet]. aleris.dk. [cited 2022 Nov
27]. Available from: https://www.aleris.dk/en/hospital-services/pectus-excavatum/faq/risks-of-nuss-procedure/ - Cohen NS, Goretsky MJ, Obermeyer RJ. Bleeding at Removal of Nuss Bar: Rare
But Sometimes Significant. J Laparoendosc Adv Surg Tech A. 2018
Nov;28(11):1393–6. - Notrica DM, McMahon LE, Johnson KN, Velez DA, McGill LC, Jaroszewski DE. Lifethreatening hemorrhage during removal of a Nuss bar associated with sternal
erosion. Ann Thorac Surg. 2014 Sep;98(3):1104–6. - Mao YZ, Tang S, Li S. Comparison of the Nuss versus Ravitch procedure for pectus excavatum repair: an updated meta-analysis. J Pediatr Surg. 2017
Oct;52(10):1545–52. - Activity after Nuss procedure: Restrictions [Internet]. aleris.dk. [cited 2022 Nov
27]. Available from: https://www.aleris.dk/en/hospital-services/pectus-excavatum/faq/activity-after-nuss-procedure/ - Pilegaard HK. Nuss technique in pectus excavatum: a mono-institutional experience. J Thorac Dis. 2015 Apr;7(Suppl 2):S172–6.
- Jung Y, Yi E, Lee K, Chung JH, Cho S, Lee S. Surgical versus Vacuum Bell Therapy
for the Correction of Pectus Excavatum: A Comparison of 1-Year Treatment Outcomes. J Chest Surg. 2021 Dec 5;54(6):473–9.